Blood Bank
The main purpose of the blood bank is to match blood products from donors to recipients who need the blood products. It is a complex subject that breaks down simply when you understand larger macro components of the immune system, and finer details of antigens and antibodies. It’s also crucial to understand testing reagents and why certain tests are used to prevent transfusion reactions.
Blood bank is a field that has evolved through a bit of trial and error. In the early days of blood transfusion there would be transfusion reactions after doctors thought the blood had been matched. This led to more research and ultimately a greater understanding of blood.
If you’ve gone through the hematology section, you’ll understand how complex red blood cells are. Blood banking brings to light another layer of complexity of red blood cells, the antigens that they possess.
The most simple and basic place to start is ABO blood typing. Everyone inherits their blood type from their parents, and each parent passes either the A, B, or O blood type resulting in 4 possible phenotypes and 6 genotypes.
| Phenotype | Genotype |
| A | AA, AO |
| B | BB, BO |
| AB | AB |
| O | OO |
What does it mean to be A, B, AB, or O blood type?
The phenotype of blood a person has is related to the antigens present on their red cells. A person with blood type A will have A antigen on their red cells. A person with blood type B will have B antigen on their red cells. A person with blood type AB will have A and B antigens on their red cells. A person with blood type O won’t have A or B on their red cells.
Conversely, a person will make antibodies naturally to red cell antigens they don’t have. Most of the time to create an antibody you need to be exposed to some sort of antigen but this isn’t the case with ABO blood antigens. A person with blood type A will make antibodies to type B red cells. A person with blood type AB will not make antibodies to A or B. A person with blood type O will make antibodies to both A and B red cells. ABO antibodies are generally IgM.
Perspective Note
There are around 600,000 to 1 million ABO antigenic sites on a single RBC.
Nerdy Note
We take the ABO blood groups for granted now but they were discovered only a little over one hundred years ago. Karl Landsteiner (1868-1943), was an Austrian physician who discovered the ABO blood groups around the year 1900. He mixed blood and serum of scientists in his lab and found some agglutinated and some did not. He then proposed it was this agglutination that caused transfusion reactions.
What’s an IgM antibody?
There are different basic classes of antibodies based on their structure. We’ll only talk about two types here, IgG and IgM. IgG antibodies have a Y shape, one arm, and two binding sites, IgM have a pentamer shape, 5 arms, and have ten binding sites. IgG antibodies are much smaller than IgM antibodies and IgG are able to cross the placenta during pregnancy (more on this later).
So, a patient who needs a blood transfusion must get the correct type of blood or a serious reaction could take place due to antibody activation. For example if a person with type A blood is transfused with type B blood, a serious reaction will take place because the patient makes IgM antibodies to type B red cells. The type B red cells are viewed as a foreign intruder. Ok but why doesn’t your immune system just remove the foreign cells? Why can transfusion reactions be deadly?
The acute hemolytic reactions caused by ABO discrepancies can be fatal because of how strongly certain systems are activated. IgM molecules activate the lysing mechanism complement leading to rapid intravascular hemolysis. IgG molecules do not activate complement as readily as IgM and tend to activate extravascular hemolysis (still serious but less so than intravascular hemolysis). In addition, each red cell wrongly transfused to a patient has hundreds of thousands of antigens which bind to the patients IgM molecules which sound the alarm in a major way.
It is also important to know how the ABO antigens look on a molecular level. They are a bit like legos, and the ABO pieces are actually sugars. Glycosyltransferases, which is a fancy word to describe a molecule that adds a sugar to something, are coded from the genes H, A, and B. There are all types of glycosyltransferases and these three genes code for three different glycosyltransferases which will then attach a sugar to the red cell which we refer to as the antigen.
The H glycosyltransferase will attach a fucose first, then the A or B sugars will attach depending on the person’s blood type (AB blood type people will have A and B sugars on the same red cell). The A sugar is N-acetyl-D-galactosamine, and the B sugar is D-galactose. The fucose attached by the H glycosyltransferase is necessary for the A and B sugars to attach, without it, they will not attach. So what if a person doesn’t have a properly functioning H gene?
More than 99.99% of the population codes for a functioning H gene but there is always an exception to the rule! There is another allele called ‘h’ which doesn’t code for a glycosyltransferase. You get one H gene from both mom and dad and if both happen to be ‘h’ you will have a rare phenotype called Bombay. Bombay phenotypes may have normal functioning A or B genes but without the H gene, A and B sugars can’t attach. People with the Bombay phenotype cannot even receive type O blood because they make anti-H immunoglobulins.
Now that we have a basic idea of ABO antigens we can touch on another important concept, ABO subgroups. It would be nice if it was as simple as A, B, or O but due to genetic complexity there can be variations.
A1 and A2 RBCs:
The A subgroups A1 and A2 account for 99% of patients with type A blood. Among the 99%, 80% are A1 or A1B, and 20% are A2 or A2B.
The difference between A1 and A2 is not structural but quantitative. An A1 individual will have about 1 million A type antigens on each RBC; whereas, an A2 individual will have about 265,000 per RBC. Why the discrepancy? It has to do with a mutation in the glycosyltransferase. The A1 is stronger and will convert most H antigen sites to A sites. The A2 converts less of the sites. So how is this tested for, and why is it important?
There is a reagent used in blood banking made from the plant Dolichos biflorus that agglutinates A1 cells but not A2. It is important to be able to distinguish between A1 and A2 phenotypes because some A2 patients make antibodies to A1 (anti-A1). About 5% of people with A2 blood and about 25% of people with A2B blood make anti-A1. So the Dolichos biflorus reagent is valuable because in a forward typing, a patient with A2 red cells will test positive with anti-A (the standard test) but test negative with anti-A1 (Dolichos biflorus).
Dolichos biflorus reagent is referred to as a lectin, and can be referred to as anti-A1 or anti-A1 lectin. Another important lectin in blood banking is Ulex europaeus, which binds H antigen and is useful in detecting a patient with the Bombay phenotype.
Forward typing and reverse typing:
The two most common tests used in the blood bank are the forward typing and reverse typing tests.
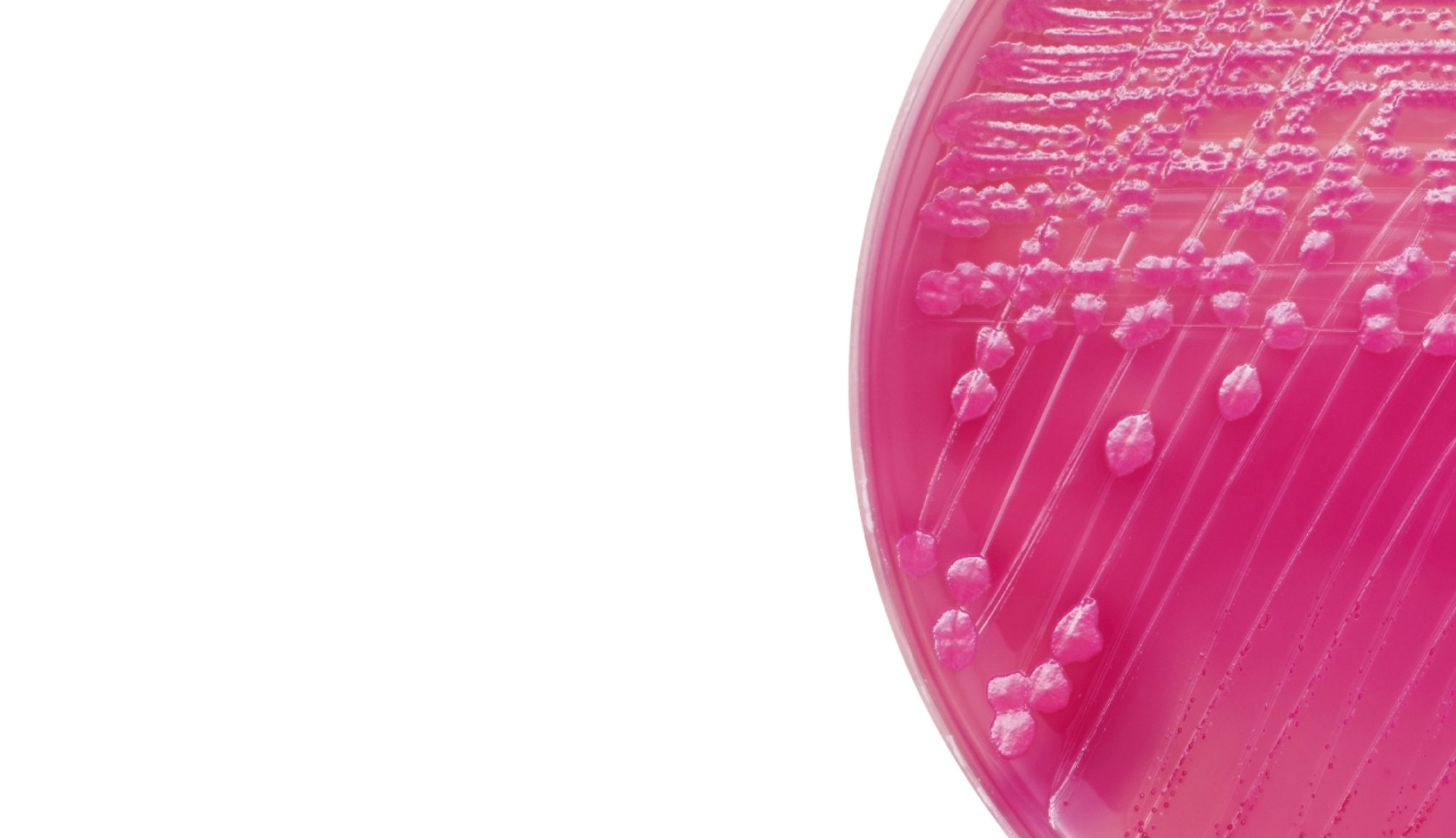
Forward typing uses commercial antisera (anti-A and anti-B) and patient red blood cells. A suspension of 2-5% patient RBCs are made and antisera is added to individual tubes. The degree of agglutination will tell you the ABO antigens present on that patients RBCs.
Reverse typing uses commercial red blood cells (A1 and B cells) and patient serum. The commercial RBCs are added to the patient serum and the individual tubes are checked for agglutination. A positive test indicates the presence of the antibody.
Agglutination scores can be 0, 1+, 2+, 3+, or 4+. The higher the number the more agglutination. For ABO testing, forward and reverse typing are inversely correlated. For example if a patient has A antigen on their red cells, they won’t make anti-A. However, in some cases the forward and reverse typing will not match up and you can have a discrepancy.