Microbiology
In microbiology, there is a lot of information to remember! If you have a system to remember the information, it is much easier to build your knowledge base. In this section there are six flowcharts and three tables to help you organize the different types of bacteria, media, and tests and a few other tips for remembering commonly seen pathogens and tests. Nothing beats hands on experience in the clinical microbiology lab but being able to quickly remember and not have to reference the results of tests can be really helpful for developing a deeper understanding of the subject and impress senior members of the lab as well. Let’s get started!
The six flow charts we’ll be discussing are:
1. Gram positive (G+), catalase positive (+) cocci
2. Gram positive (G+), catalase negative (-) cocci
3. Gram positive (G+) bacilli
4. Gram negative (G-), lactose fermenting bacilli
5. Gram negative (G-), non-lactose fermenting bacilli
6. Anaerobes
We’re going to focus on the bacteria, media, and tests most commonly seen in the clinical lab (and seen on tests). Let’s start with the gram positive (G+) cocci.
What is a gram stain?
A gram stain is a test where gram positive (G+) bacteria can be distinguished from gram negative (G-) bacteria by using dyes. Bacteria from either a plate or a broth solution will be added to a microscope slide. The slide will be dried and then a crystal violet stain will be applied. Iodine will be added to fix the crystal violet dye and then the slide will be washed with alcohol. G+ bacteria will hold the stain at this step whereas G- bacteria will lose the stain at this step mainly due to the different cell wall structures each possess. A counter stain of safranin will then be applied, and the G- bacteria will hold onto this stain. The slide is rinsed with DI water and dried and it’s ready for the microscope! It’s a simple, routine, and fundamental (at least for now) test of the microbiology lab.
Typical gram stain procedure:
Crystal violet – 1 minute
Iodine – 1 minute
Alcohol wash
DI water wash
Safranin counter stain – 30 seconds
DI water wash
Dry slide
Under the microscope G+ bacteria will look dark purple, and G- bacteria will have a pinkish-red color. Not all bacteria will pick up the stain, there are always exceptions to the rule. The test is quick to run, and can potentially give a lot of information in a short amount of time. Remember a lot of tests in the microbiology lab require at least overnight incubation.
Ok back to G+ cocci. What are cocci? A cocci refers to any bacteria that has a round or spherical shape (think a grape). Other types of bacterial shapes are bacilli (rods), and spirochetes (spirals). Ok let’s jump into the G+, catalase + flow chart:

Catalase Test:
The catalase test is used on a wide variety of bacteria. It’s a common enzyme found in many living organisms. In this instance, it will tell you if you have a Staphylococcus (catalase +) or a Streptococcus bacteria (catalase -). The catalase test is run by adding hydrogen peroxide to the bacteria on a slide. If bubbles of oxygen are seen, the bacteria contains catalase and the test is positive. If no reaction occurs, the test is negative, and in this instance would point to a Streptococcus (Strep) bacteria. We’ll get to Strep in the next flow chart. Ok so for a G+, catalase + bacteria, the next test to run is coagulase.
Coagulase Test:
What is coagulase? Coagulase is an enzyme produced by Staph aureus that converts fibrinogen to fibrin (the coag factor!) Staph aureus can produce coagulase in two forms, bound (aka clumping factor) and free. There are two types of coagulase tests, the slide test and the tube test. The slide test is rapid and detects bound coagulase but is less reliable than the tube test which involves a longer incubation. The slide test is run by adding a drop of reagent coagulase plasma (usually rabbit plasma with EDTA) to the bacteria on a slide. If the sample is coagulase + the sample will agglutinate and clump together. If it’s coagulase -, it will stay clear and have no clumping. There are always exceptions to the rule, and there are Staph strains other than Staph aureus that are coagulase positive but for the sake of clarity and to avoid confusion they’re not listed. In addition, about 10-15% of Staph aureus bacteria won’t have bound coagulase (clumping factor), thus the need for the tube coagulase test which can detect free coagulase. The coagulase tube test involves a 4-hour 35C incubation, and an 18-24 hour incubation. Both must be negative to rule out S. aureus. The test must be read by the 4-hour mark. Why is this? S. aureus can produce fibrinolysis products that break down the clot it may have previously helped to form. Bacteria are quite sophisticated! This is important because at 4 hours you may have a positive sample while later or at 18-24 hours it may be negative because S. aureus broke down the clot.
Oxidase Test:
If your sample is coagulase negative the next tests to run are the oxidase and bacitracin tests. An important thing to remember is these flow charts are not how a clinical lab runs tests. They’re merely a memory tool for distinguishing bacteria. Sometimes a test question will only give you certain results, for example it would give you bacitracin results but not oxidase or vice versa, so it’s important to know both. A lab may only run one of the tests. The oxidase test detects the enzyme cytochrome c, which is part of electron transport and nitrogen metabolism in some bacteria. A positive test will give you a purple color and negative will be colorless. This is a common test usually run with paper strips with a specific chemical coating.
Bacitracin Test:
The bacitracin test is more commonly used to differentiate strains of Strep but it’s useful with Staph too. Bacitracin is an antibiotic that interferes with cell wall synthesis in some bacteria. The test is run by placing a bacitracin disc on a sheep blood agar (SBA) plate that has the bacteria in question growing on it. After incubation, if the bacteria is sensitive to bacitracin you will see a ring around the disc where no bacteria is growing. If the bacteria is resistant, the bacteria will be growing right next to the disc. Antibiotic discs are a common theme in the microbiology lab. So if the oxidase test is positive or if the culture is sensitive to bacitracin you have a Micrococcus bacteria, which isn’t Staph! Micrococcus is a small bacteria that is rarely implicated in disease. If the oxidase test is negative or the bacitracin is resistant, you have a coagulase negative Staph which can be further broken down by a novobiocin test.
Novobiocin Test:
Novobiocin is an antibiotic that inhibits bacterial DNA gyrase. The novobiocin test is run just like the bacitracin test but with a novobiocin disc. A sensitive test will give you Staph epidermidis, and a resistant test will give you Staph saprophyticus.
Other notes for G+ cocci:
S. aureus:
Produces hyaluronidase which damages the intercellular membrane of tissues Associated with toxic shock syndrome
S. epidermidis:
Can produce a slime that helps it attach to catheters and other medical devices Associated with nosocomial infections Can be methicillin resistant
CNA agar:
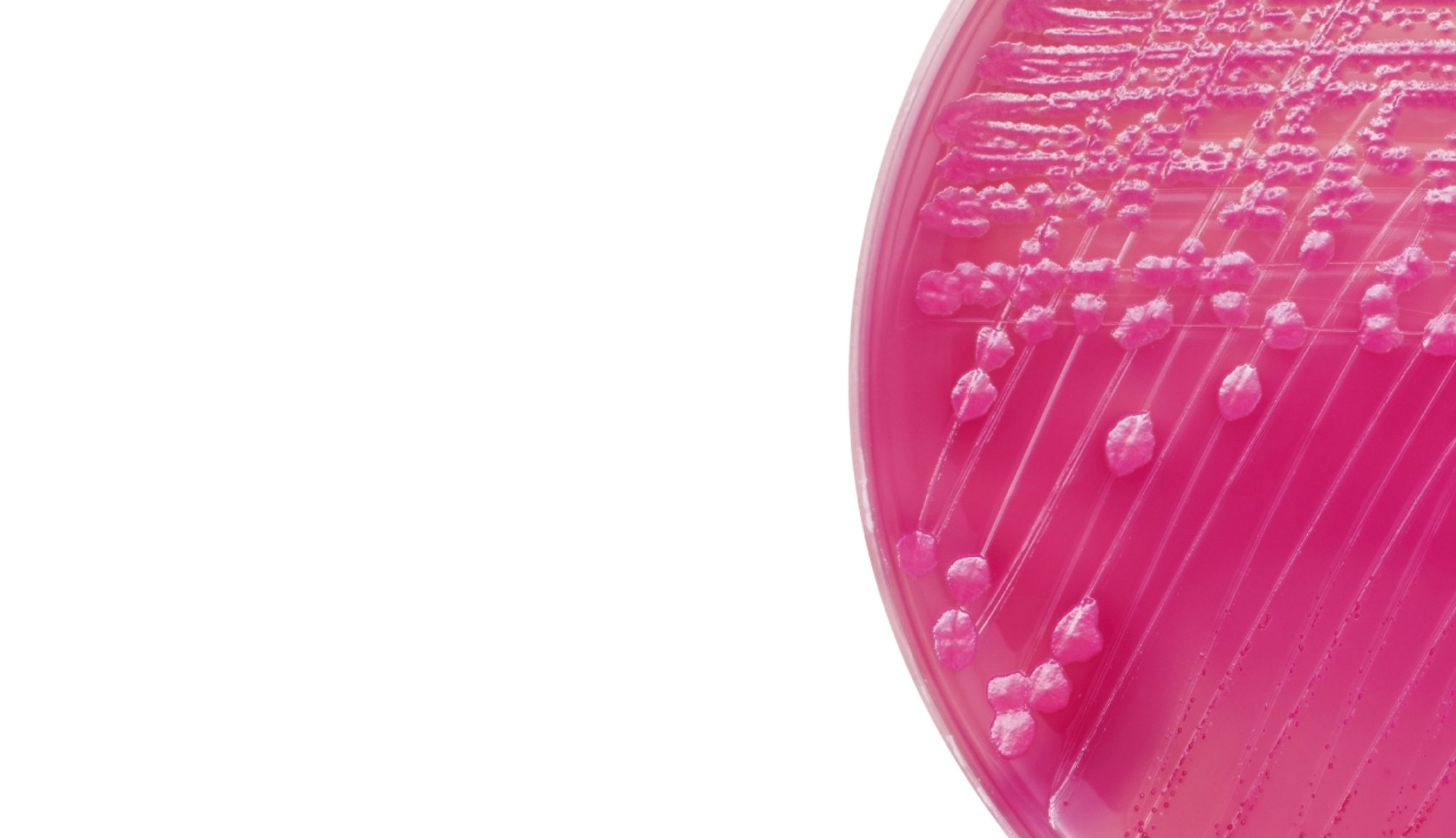
CNA agar (Columbia agar with colistin and nalidixic acid) is selective for Staph aureus and G+ cocci. The antimicrobials colistin and nalidixic acid inhibit G- bacteria.
Study Tip
The best way to remember these flow charts is to draw them over and over again. Take out a blank piece of paper and write them out a few times everyday until it’s second nature. Once you’re comfortable with the flow chart, start writing the conditions, diseases, and other standout features associated with each organism.
Nerdy note
Staph aureus has an enzyme coagulase that is known through a series of reactions to convert fibrinogen to fibrin. It’s hypothesized that Staph aureus uses the created fibrin to build a capsule and avoid being destroyed by the immune system. Whoa! Sneaky!