Acute myeloid leukemia (AML)
Acute myeloid leukemia (AML):
It’s all in the name. Acute is going to indicate the condition has a more sudden onset than a chronic condition. Acute is also going to indicate that more cells immature in development will be present. Myeloid tells you this is effecting myeloid cells like granulocytes, RBCs, and platelets. Leukemia tells you the cells are effecting the bone marrow and peripheral blood. Leukemia is also going to indicate that a certain cell type is growing rapidly and is out of control.
The main thing to look for in AML is an increased myeloid blast count that is ≥20% in the peripheral blood and bone marrow. AML can present with a very high or very low WBC count so be aware of this. AML generally presents with anemia, thrombocytopenia, and granulocytopenia due to the marrow being overtaken by leukemic cells. Imagine all of a sudden there are multiple clones of yourself in your house, and eventually there are 200 clones of you all trying to squeeze in your house. This is going to effect your normal function, and you won’t be able to get anything done. This is analogous to what leukemia can do to your bone marrow.
AML is a wide spectrum of conditions because it includes all the myeloid cell types. AML breaks down into many sub categories based off of cell type, morphology, cell staining, immunophenotype (CD antigens), and genetics. The terminology for diagnosing AML is constantly evolving because sequencing, molecular techniques, computing power, and human innovation are improving the specificity of the diagnoses. We are getting closer to understanding these complex conditions and at the same time developing new treatments for them.
Since the terminology is a bit of a moving target there are unfortunately multiple classification systems to be aware of. The two major systems are the French-American-British classification system (FAB), and the World Health Organization (WHO) classification system.
Study Tip
Be aware that the FAB classification system actually calls for a ≥30% blast count in the peripheral blood or bone marrow to diagnose AML; whereas, the WHO classification requires ≥20%.
The French American British classification system (FAB):
Although becoming more obsolete, the FAB terminology is still used by some. It divides AML into eight subgroups (M0-M7) mostly based off of cell type, morphology, cytogenetics, and cell staining results seen on peripheral smears and bone marrow aspirate smears. It was introduced in 1976, the table below outlines the basics.
| Classification | Name | Cytogenetic association |
| M0 | AML without differentiation | |
| M1 | AML with minimal maturation | |
| M2 | AML with maturation | t(8:21) |
| M3 | Acute promyelocytic leukemia (APL) | t(15:17) |
| M4 | Acute myelomonocytic leukemia (AMML or AMMoL) | inv(16) |
| M5 | Acute monocytic leukemia or acute monoblastic leukemia | |
| M6 | Acute erythroid leukemia | |
| M7 | Acute megakaryoblastic leukemia |
Study Tip
M0-M3 is basically a progression in maturity. It’s easy to remember that M0 is the most immature, and each step up the cells will become more mature up to M3. M4-M7 deal with specific cell types.
Memory Trick
Use the phrase “My Mono-Mono-Red-Mega” to remember the basis for M4-M7.
4-My Mono (myelomonocytic)
5-Mono (monocytic)
6-Red (erythroid)
7-Mega (megakaryoblastic)
M0 (AML without differentiation):
In M0 you can’t distinguish between myeloid cells and lymphoid cells morphologically (under the microscope) or cytochemically (staining), hence the name AML without differentiation. The use of flow cytometry or immunophenotyping is necessary to identify a myeloid specific antigen.
M1 (AML with minimal maturation):
M1 is defined by >90% myeloblasts. Most of the cells are very immature.
M2 (AML with maturation):
M2 is defined by 20-90% myeloblasts. Cells are still immature but more mature than M1.
M3 (Acute promyelocytic leukemia (APL)):
M3 is defined by abnormal promyelocytes. Also about 15% of patients have a chromosomal translocation between chromosomes 15 and 17 t(15:17). Patients with this abnormality respond to the treatment All-transretinoic acid (ATRA) which forces the maturity of promyelocytes. It is common to see Auer rods in this sub-type of AML. The presence of Auer rods is an important clue for distinguishing AML from ALL.
M3 can also be associated with disseminated intravascular coagulation (DIC). The primary granules in the promyelocytes contain a thromboplastic substance that can cause clotting, so when these cells are over proliferating they can cause coagulation problems.
M4 (Acute myelomonocytic leukemia (AMML or AMMoL)):
M4 is defined by both myeloid and monocytic differentiation. To me, this is poorly named because monocytes fall under the myeloid classification. M4 has monocytic and granulocytic differentiation. The chromosomal abnormality inv(16) is associated with M4. Monocytes can also be detected cytochemically using a nonspecific esterase stain. This stain can be helpful in determining the percentage of monocytic cells.
M5 (Acute monocytic leukemia or acute monoblastic leukemia):
M5 is defined by an increase in monocytic cells. M5 can be further broken down into M5a and M5b. M5a, acute monoblastic leukemia is defined by >80% monoblasts in the bone marrow or peripheral blood. M5b is associated with >20% monoblasts in the bone marrow or peripheral blood. The non-specific esterase stain can be especially useful in this sub-type.
M6 (Acute erythroid leukemia):
M6 is defined by an increase in erythroid precursor cells. It is defined as ≥50% erythroid precursors and ≥20% myeloblasts in the bone marrow. M6 will stain strongly with the Periodic acid-Schiff (PAS) stain.
Pure erythroleukemia is defined as >80% erythroid precursor cells in the bone marrow. It is also known as Di Guglielmo syndrome.
M7 (Acute megakaryoblastic leukemia):
M7 is defined by an abnormal amount (usually ≥50%) of megakaryoblasts in the bone marrow.
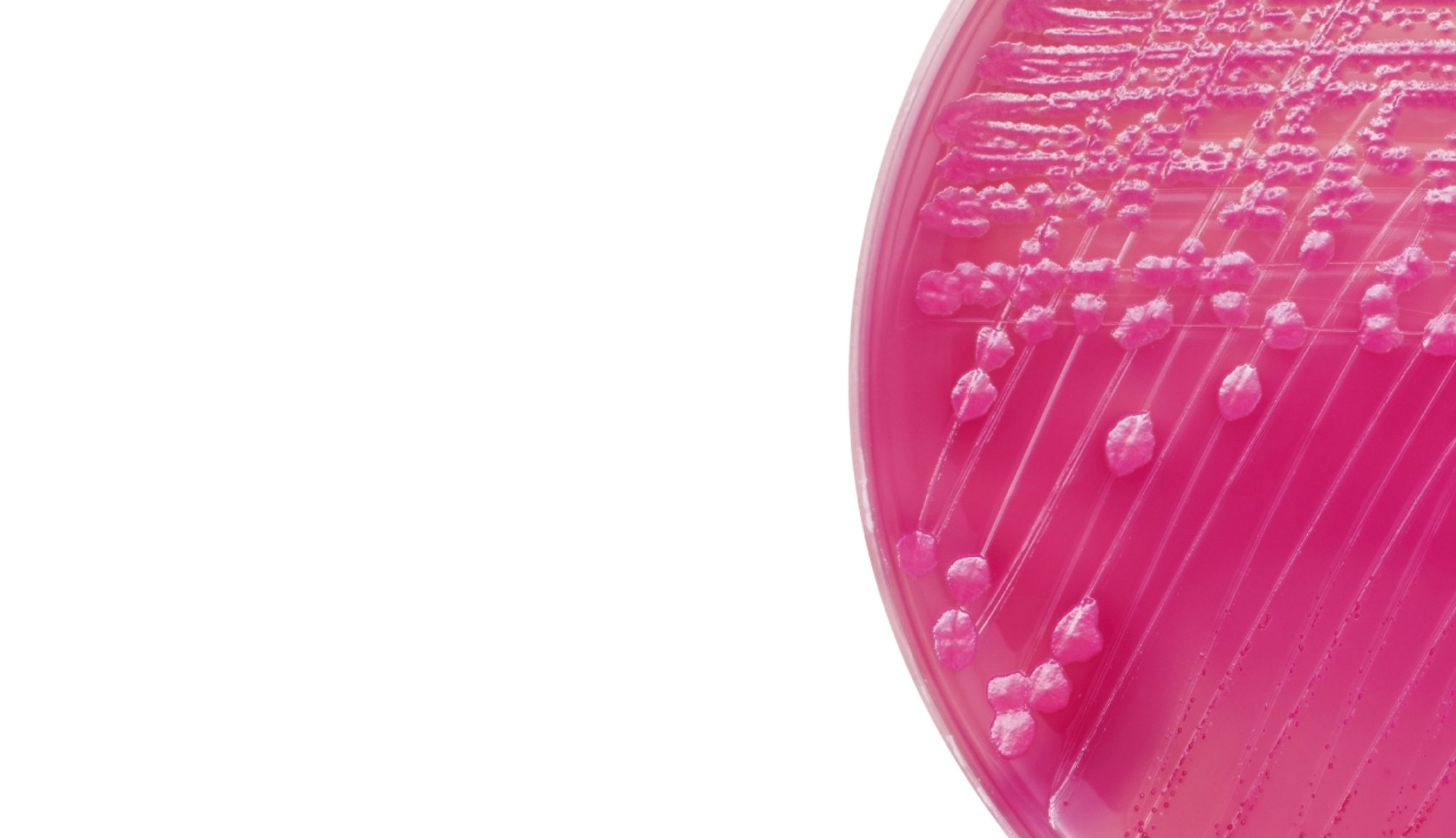
Cytochemical staining (cell staining), although becoming less useful can still be helpful to know. There are a lot of stains that will stain blast cell lines weakly or give a variable result. The table below only lists stains of most importance.
| Stain | M0 | M1 | M2 | M3 | M4 | M5 | M6 | M7 |
| Myeloperoxidase | - | + | + | + | + | |||
| Sudan Black B | - | + | + | + | + | |||
| Chloroacetate esterase | - | + | + | + | ||||
| Nonspecific esterase | - | + | + | |||||
| Periodic acid-Schiff | - | + | + |
The World Health Organization (WHO) classification of tumors of the hematopoietic and lymphoid tissues is a project that began in 1995. It is a system that is constantly evolving and was recently updated in 2016 to mostly reflect progress made in genetics. For AML, it breaks down into five main groups.
1. AML with recurrent genetic abnormalities:
t(8:21), t(15:17), and inv(16) all fall into this category amongst many other genetic abnormalities.
2. AML with multi-lineage dysplasia:
This category is defined by ≥20% blasts in the peripheral blood or bone marrow and >50% dysplasia in two or more myeloid cell lines.
3. AML and myelodysplastic syndromes (MDS) that are therapy related (t-AML and t-MDS):
Chemotherapy, radiation, and other treatments can cause mutations and unique variations of AML to arise.
4. AML not otherwise categorized:
This category includes parts of M0, M1, M2, M4, M5, M6, and M7. This is a broad category.
5. Acute leukemias of ambiguous lineage:
This can include leukemias with cells that express both myeloid and lymphoid characteristics. The more granular diagnostic tools are showing there are many ambiguous combinations of acute leukemias.